The July 29th edition of the Providence Journal featured a front page story about the swimming program for inner-city youth that is organized by Providence Community Health Centers and held at Pods Swimming in East Providence. The program is supported by a grant from the USA Swimming Foundation.
In these classes, children learn the elementary backstroke, how to float, and other valuable water safety skills. There are two four-week sessions of classes, held in July and August. This year, more than 40 children have registered for the classes.
The Providence Journal story, which is subscription only, is linked here: https://www.providencejournal.com/story/news/local/2021/07/28/some-providence-children-learning-swim-some-arent/5391533001/












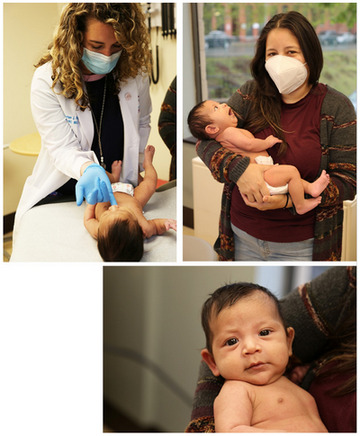 Breastfeeding has many proven benefits for both the newborn baby and mother. Providence Community Health Centers is now offering lactation health support provided by Kristen Hylan, MSN, FNP-BC, who is an International Board-Certified Lactation Consultant.
Breastfeeding has many proven benefits for both the newborn baby and mother. Providence Community Health Centers is now offering lactation health support provided by Kristen Hylan, MSN, FNP-BC, who is an International Board-Certified Lactation Consultant.
